- About ASOPRS
- Membership
- Symposia
- Fellowships
- OPS Community
Eyelid Skin Cancer
What are the causes? Excessive exposure to sun is the single most important factor associated with skin cancers of the face, eyelids, and arms. Fair-skinned people develop skin cancers far more frequently than darker-skinned people. Skin cancers may also be hereditary. The most common types of periocular (eye area) skin cancers are basal cell carcinoma and squamous cell carcinoma. Either may appear as a painless nodule, or as a sore that won’t heal. The skin may be ulcerated, or there may be bleeding, crusting, or the normal eyelid structure may be deformed. The eyelashes may be distorted or missing. Melanomas arise from the pigment-producing melanocytes. This is a less common but more serious form of skin cancer. A mole that bleeds or becomes tender, or one that changes is size, shape, or color, should be evaluated by a physician. Sebaceous gland carcinoma arises from the oil glands in the skin. This is also a more serious form of skin cancer. It may appear as a thickening of the eyelid, or as persistent eyelid inflammation. Basal cell skin cancers enlarge locally and rarely spread (metastasize) to other parts of the body. Left untreated, they will continue to grow and invade surrounding structures. Squamous cell carcinomas, melanomas, and sebaceous gland carcinomas can metastasize to other parts of the body through the bloodstream or lymphatic system. Prompt, aggressive treatment is necessary because of the risk of early spread. Treatments Your doctor may recommend Mohs surgery, which is a technique where the lesion is removed layer by layer with same-day microscopic confirmation. A dermatologist specially trained in the technique performs Mohs surgery, and the oculofacial plastic surgeon repairs the area once the cancer is removed. Alternatively, your surgeon may elect to remove the cancer using frozen sections. In this instance, the surgeon removes the lesion with a small margin of normal tissue. The specimen is quickly frozen and the pathologist examines the tissue to determine if the entire tumor has been removed. Once this is confirmed, the area is repaired. How the area where the skin cancer was removed is reconstructed depends on the size of the defect left behind. Smaller defects can be repaired by suturing the edges together. Larger areas may require local flaps or free skin grafts to close them. Radiation may be useful for patients who cannot tolerate surgery, or in addition to surgery in more aggressive types of skin cancers. Early and complete removal of eyelid skin cancers is vital to reduce the chance of a recurrence, and to reduce the risk of spread to other parts of the body. Careful follow-up after surgery is necessary to look for recurrence and to look for new cancers so they can be treated promptly. Risks and Complications Your surgeon cannot control all the variables that may impact your final result. The goal is always to improve a patient’s condition but no guarantees or promises can be made for a successful outcome in any surgical procedure. There is always a chance you will not be satisfied with your results and/or that you will need additional treatment. As with any medical decision, there may be other inherent risks or alternatives that should be discussed with your surgeon. |

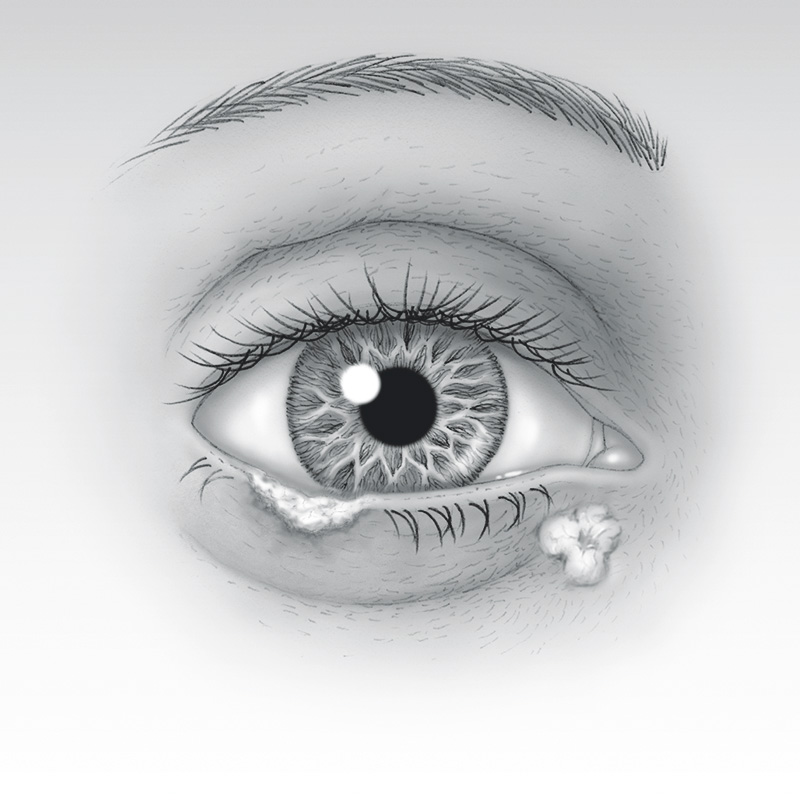 The outer layer of skin is called the epidermis. Epidermal cells include flat squamous cells, round basal cells, and pigment producing melanocytes. The dermis is the deeper layer of skin and contains the hair follicles, oil and sweat glands, and blood vessels. Skin cancers can arise from any of these skin cells. A biopsy is usually required to confirm the diagnosis of skin cancer.
The outer layer of skin is called the epidermis. Epidermal cells include flat squamous cells, round basal cells, and pigment producing melanocytes. The dermis is the deeper layer of skin and contains the hair follicles, oil and sweat glands, and blood vessels. Skin cancers can arise from any of these skin cells. A biopsy is usually required to confirm the diagnosis of skin cancer.